45yr old male with acute pancreatitis
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
NAME : ANKITHA
ROLL NO : 78
This is a case of a 45 year old male, carpenter by occupation came to OPD with chief complaints of:
1. Pain abdomen since 2 days
2. Vomitings since 2 days
3. Constipation since 3 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 day ago then he developed pain in the abdomen- in epigastric region.
It was sudden in onset, gradually progressive.
Pain more after eating food and on lying in supine position.
Pain relieved on sitting , on bending forward.
Yesterday he went to a local rmp and took medication but pain did not subside so came to our hospital today
-H/O 3 episodes of Vomiting yesterday after eating food, food as content, non bilious, non projectile, not blood tinged.
-Constipation since 3 days
Last binge of alcohol consumption 2days ago.
No H/O fever, cough, cold, shortness of breath, loose stools, giddiness , burning micturition
PAST HISTORY:
H/O similar complaints 2 years ago- diagnosed as Acute pancreatitis, treated at KIMS Narketpally
No significant family history
SYSTEMIC EXAMINATION:
PER ABDOMEN :
Inspection :
Abdomen is scaphoid
Umbilicus is central
All quadrants are moving equally with respiration
No sinuses , engorged veins, visible pulsations .
Palpation :
No local rise of temperature
Tenderness present in epigastric region
Liver and Spleen - Not palpable
Percussion : Tympanic note heard over the abdomen.
Fluid thrill absent
Shifting dullness absent
Auscultation :
Bowel sounds are heard.
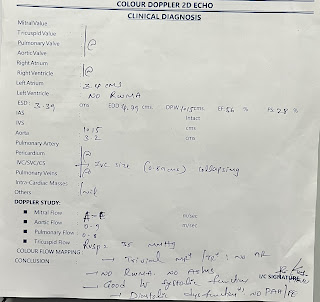
CARDIOVASCULAR SYSTEM :
Inspection:
Shape of chest is elliptical.
No raised JVP
No visible pulsations, scars , sinuses , engorged veins.
Palpation :
Apex beat - felt at left 5th intercostal space
No thrills and parasternal heaves
Auscultation :
S1 and S2 heard.
RESPIRATORY SYSTEM:
Inspection :
Shape- elliptical
B/L symmetrical
Both sides moving equally with respiration .
No scars, sinuses, engorged veins, pulsations
Palpation:
Trachea - central
Expansion of chest is symmetrical.
Vocal fremitus - normal
Percussion: resonant bilaterally
Auscultation:
bilateral air entry present
Wheeze present
CENTRAL NERVOUS SYSTEM:
Conscious,coherent and cooperative
Speech- normal
No signs of meningeal irritation.
Cranial nerves- intact
Sensory system- normal
Motor system:
Tone- normal
Power- bilaterally 5/5
Reflexes Right Left
Biceps ++ ++
Triceps. ++. ++
Supinator ++ ++
Knee. ++. ++
Ankle ++. ++








Comments
Post a Comment