70Year Old Male with Altered Sensorium
Timeline:
25 days ago:The patient was apparently asymptomatic 25 days ago when he went on a sudden alcohol binge for a couple of days following which he developed cough assosciated with sputum (scanty, non foul smelling, non sanguinous) and shortness of breath that could initially be classified under Class 2 NYHA(SOB with ordinary activity, slight limitation of physical activity) but gradually progressed to class 4(SOB at rest, severe limitation of physical activity). He also had burning sensation of the oral cavity that he recalls to have begun around the same time.
Following these complaints, the patient was taken to a nearby Government hospital, where he was treated symptomatically with mouth guard gel and chlorhexidine mouth wash.
22 days ago: The patient was shifted to another local hospital where a chest X Ray was done and he was told he has viral pneumonia of the right lung.
5 days ago: The patient was brought to our hospital by his wife who said that she noticed a change in his responsiveness and slurring of speech that began 5 days ago. The patient presented to the casuality ward with some drowsiness, but he was arousable.
On examination of his oral cavity, multiple erythematous lesions are seen over his hard palate
PAST HISTORY
No similar complaints in the past.
No H/o DM ,HTN, TB, Asthma, epilepsy,CAD
History of surgeries or blood transfusion:
History of transfusion of two units of FFP
Central line for dialysis on 7th January.
FAMILY HISTORY
No history of similar illnesses among immediate family members.
The patient lost his first wife to an unknown illness 30 years ago. He has 2 daughters with his second wife.
No history of CKD, DM,HTN,CVA, TB, Asthma or CAD among his immediate family members.
PERSONAL HISTORY
Diet: Mixed
Appetite: decreased recently
Sleep:Adequate
Bowel and bladder:Decreased urine output
No known drug allergies
He consumes 150ml of Alcohol every other day, his last intake was 25 days back.
Tobacco usage since 30 years.
GENERAL EXAMINATION
Patient is conscious, not coherant or cooperative, not oriented to time, place and person. He appears confused and irritated.
Moderately built and nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema.
VITALS:
Temperature: febrile on arrival
PR: 87 bpm
BP: 120/70 mmHg
RR: 24 cpm
SpO2: 98% with 4L of O2
GRBS: 229mg/dl
SYSTEMIC EXAMINATION:
CNS:
Higher mental functions-
Speech: slurred
Cranial nerve functions - Intact.
Sensory system- sensitive to pain, touch , vibration and temperature.
Respiratory system:
Inspection:
trachea central in position.
On percussion:dullness on right upper lobe
On auscultation:bilateral air entry present,NVBS
B/L Creptititions heard
CVS:
Inspection : no visible pulsation , no visible apex beat , no visible scars.
Palpation: all pulses felt , apex beat felt.
Percussion: heart borders normal.
Auscultation:S1, S2 Heard, no added murmurs.
P/A: Soft, non tender
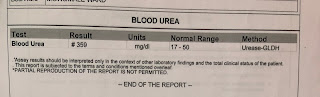
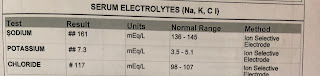
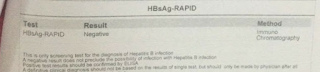
Investigations:
Blood grouping and Rh typing :
Sputum for AFB: NEGATIVE
USG Abdomen :
PROVISIONAL DIAGNOSIS:
Altered sensorium as a consequence of exacerbated uremic encephelopathy along with acute kidney injury secondary to sepsis, viral pneumonia of the right upper lobe in a 70 year old
TREATMENT:
intravenous fluid ( normal saline,ringer lactate)
- Ryle tube feeds 100 ml milk 2 nd hourly
50 ml water hourly
1. MUCOPAIN Gel BD* 1 week
2. BETADINE mouth gargles TID* 1 week
3. Tab MVT OD* 15 days
4. Inj PIPTAZ 2.25gm TID
5. THIAMINE in 100ml normal saline TID
6. Tab AZITHROMYCIN 500mg*PO/OD
7. Inj LASIX 40mg IV BD
8. Tab Montek-LC
9. Tab ACEBROPHYLLINE
10. Tab Pulmoclear PO OD
11. Syp: Ambroxyl 15ml PO TID
12. Nebulizer with BUDECORT- 8th hourly
Duolin- 12th hourly
13. Inj HYDROCORTISONE 100mg IV stat
14. Inj VIT K 1 ampoule in 100ml NS for slow IV
Other measures: Head elevation
Vitals checked every 4hrs
O2 inhalation to maintain SpO2 greater than 94%
Monitor urinary output
GRBS every 6th hourly
Chest physiotherapy



















Comments
Post a Comment