35yr male with pancreatitis and hypertension
K.Ankitha
Rollno : 78
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
CHEIF COMPLAINTS :
Patient was brought to casuality with chief complaints of pain abdomen since 1 day
Patient was apparently asymptomatic untill yesteday afternoon . He then had Pain abdomen which was insidious in onset and gradually progressive (pain in all areas) associated with nausea and vomitings.
- C/O vomitings - 10 episodes yesterday and no vomitings today, watery in nature , non projectile, Bilious with food particles as content , non blood tinged.
- C/O Fever since 1 day - low grade,intermittent , no chills and rigor and relieved on medication (subsided now)
- C/O SOB - Insidious in onset , gradually progressing
SOB at rest - C/O abdominal distension and discomfort.
No C/O loosestools ,burning micturition , chest pain.
No similar complaints in the past.
- K/C/O Hypertension since 3 years on irregular medication (using Amlong 5mg + Aten 50mg od )
- Not a K/C/O DM/ TB/ CVA /CAD/ Epilepsy /Thyroid disorder
Diet : mixed
Appetite : normal
Sleep : normal
Bowel and Bladder : Regular
No allergies
Addictions : Regular Alcoholic since 7-8 years
(Last alcohol intake yesterday morning)
Tobacco chewing since 7-8 years
Under Aseptic conditions , from Rt knee through suprapatellar approach about 97ml of synovial fluid is aspirated and sent for investigations.
GENERAL EXAMINATION :
Patient is conscious , coherent , cooperative
Moderately built and nourished .
No signs of pallor , icterus , cyanosis , clubbing , lymphadenopathy , edema.
VITALS :
Afebrile.
PR - 98bpm
BP - 130/80 mmhg
RR - 20 cpm
SpO2 - 98% on Room air
GRBS - 213mg%
SYSTEMIC EXAMINATION :
PER ABDOMEN :
Inspection :
Abdomen is obese
Umbilicus is central
All quadrants are moving equally with respiration
No sinuses , engorged veins, visible pulsations .
Hernial orifices are free.
Palpation :
No local rise of temperature
Tenderness present in epigastrium and right hypochondrium
Liver and Spleen - Not palpable
Percussion : Tympanic note heard over the abdomen.
Fluid thrill absent
Shifting dullness absent
Auscultation :
Bowel sounds are heard.
CARDIOVASCULAR SYSTEM :
Inspection:
Shape of chest is elliptical.
No raised JVP
No visible pulsations, scars , sinuses , engorged veins.
Palpation :
Apex beat - felt at left 5th intercostal space
No thrills and parasternal heaves
Auscultation :
S1 and S2 heard.
RESPIRATORY SYSTEM:
Inspection:
Shape- elliptical
B/L symmetrical
Both sides moving equally with respiration .
No scars, sinuses, engorged veins, pulsations
Palpation:
Trachea - central
Expansion of chest is symmetrical.
Vocal fremitus - normal
Percussion: resonant bilaterally
Auscultation:
bilateral air entry present
Wheeze present
CENTRAL NERVOUS SYSTEM:
Conscious,coherent and cooperative
Speech- normal
No signs of meningeal irritation.
Cranial nerves- intact
Sensory system- normal
Motor system:
Tone- normal
Power- bilaterally 5/5
Reflexes Right Left
Biceps ++ ++
Triceps. ++. ++
Supinator ++ ++
Knee. ++. ++
Ankle ++. ++
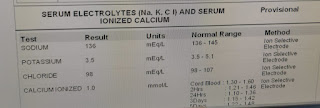
INVESTIGATIONS
Hb - 11.7g%
TLC - 11,000
Platelet - 2.0
RBC - 4.0
Impression : Neutrophilic leucocytosis
Usg abdomen : 19/03/23
21/03/23 :
22/03/23 :
23/03/23 :
PROVISIONAL DIAGNOSIS :
ACUTE PANCREATITIS secondary to alcohol With K/c/o HYPERTENSION since 3 years
With ? Septic arthritis Rt Knee joint ? Acute Gout
With ? Chronic liver disease
TREATMENT :
- Soft diet
- IV Fluids - 1 unit NS , 1 unit RL @100ml/hr
- Inj. Tramadol 1 amp. In 100 ml NS IV/TID
- (D6) Inj. Thiamine 200mg in 100ml NS IV/TID
- Inj. PANTOPRAZOLE 40mg IV/OD
- Inj. Z0FER 4 mg IV/SOS
- Inj. PCM 1gm/IV/SOS
- Tab.PCM 650mg PO/SOS
- Tab. Amlokind AT (5+50) PO OD.
- Tab.UDILIV 300mg PO/BD
- Tab. RIFAGUT 550mg PO/BD
- Tab. CHYMEROL FORTE PO/BD
- Syp. HEPAMERZ 15ml PO/BD
- Syp. LACTULOSE 15ml PO/BD
- Oint. THROMBOPHOBE for L.A
- Grbs, Vitals monitoring 4th hrly and inform sos




































Comments
Post a Comment